Firstup has released research revealing that communication failures in hospitals are directly undermining nurse engagement and operational effectiveness. The State of Nursing Communication Report surveyed 1,000 US hospital nurses between September and November 2025 to examine how workplace communication affects everything from policy compliance to daily clinical operations.
The findings reveal a fundamental disconnect between the volume of information hospitals distribute and what nurses can realistically process during their shifts. While hospitals communicate frequently with nursing staff, traditional delivery methods are proving inadequate for the realities of clinical environments. The study links these communication gaps to nurse retention, workplace stress, and patient outcomes.
The Engagement Gap: Why Messages Aren’t Landing
Firstup positions the research, which included full-time, part-time, and travel nurses working in hospital settings, as evidence that healthcare organizations must rethink how they reach frontline clinical staff with communications.
The survey data shows that frequency of communication does not equate to effective engagement. Nearly 70% of nurses reported receiving workplace updates several times a week or more, yet almost half described those communications as only “somewhat” relevant to their specific roles. This lack of targeted content leads to widespread message fatigue, with 67% of nurses admitting they skim or delete workplace messages at least sometimes without fully reading them.
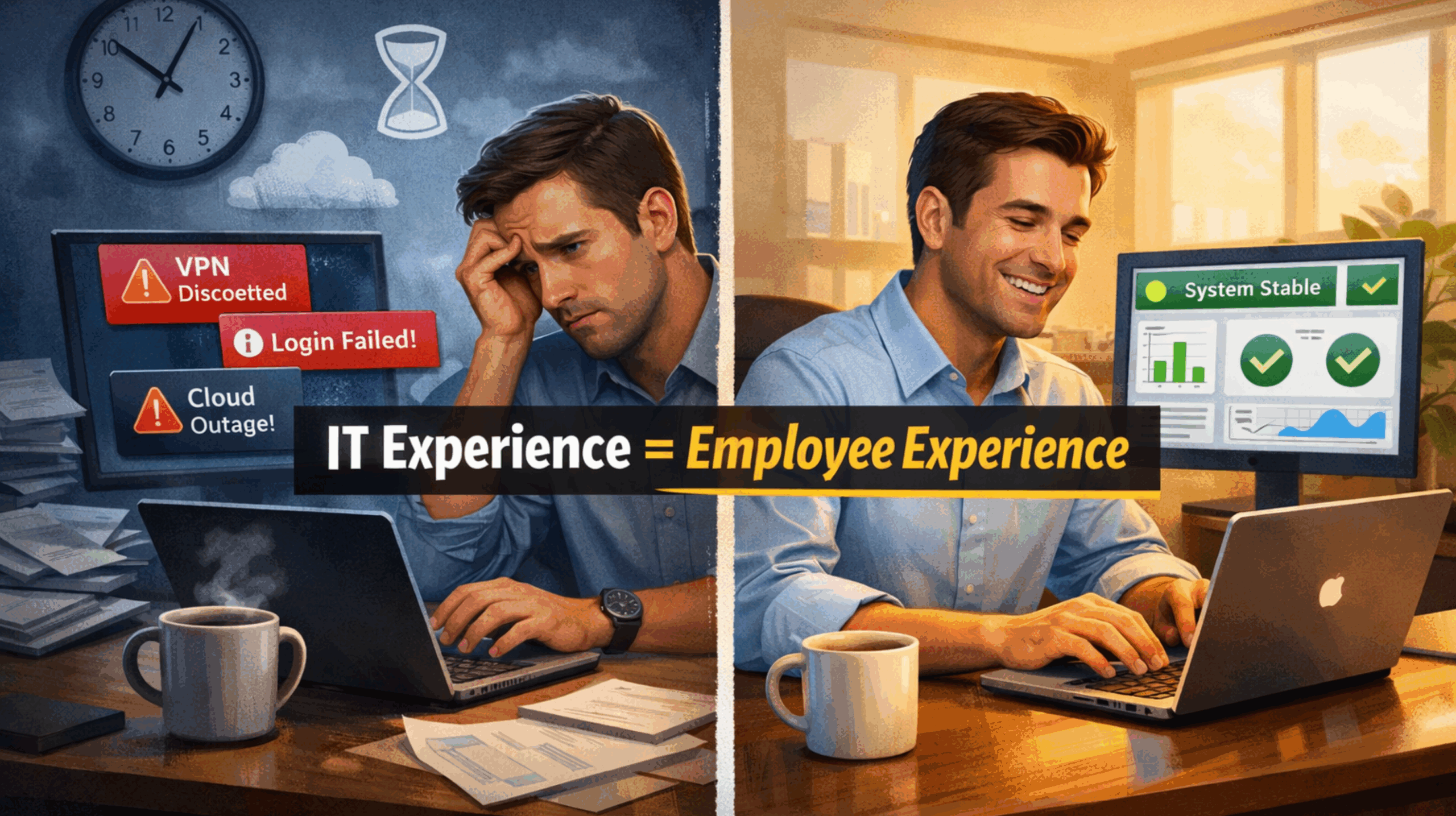
The problem extends beyond relevance to basic accessibility. Email remains the primary communication channel for 86% of hospitals surveyed, while 25% of nurses still receive paper notices. Both methods prove ineffective for clinicians who lack time to check inboxes during high-pressure shifts. One-third of respondents said they don’t have time to read updates, 19% lacked motivation, and 13% said they feel disengaged from their hospital.
This communication breakdown has tangible consequences for policy awareness. Nine in ten nurses reported learning about new policies or procedures only after they had already taken effect at least once. Nearly half said this had happened several times. Additionally, 16% of nurses had missed updates on safety protocols, and 10% had overlooked HIPAA or compliance information.
These findings indicate that confidence in existing communication systems is limited. About 48% of nurses expressed being only “somewhat confident” that their hospital’s communication efforts keep them compliant with required policies. Roughly 38% said their hospital’s communication about staffing changes, new equipment, safety protocols, and onboarding needs improvement.
The prevalence of “somewhat” in these responses shows that hospitals are falling short of the reliability standards clinical environments demand.
Patient Care and Workforce Sustainability at Risk
The study found that the consequences of poor communication extend beyond policy updates or staffing changes. The report revealed that ineffective communication directly impacts patient care quality.
A striking 81% of nurses reported experiencing patient care issues due to miscommunication or lack of communication from management. The specific impacts included inefficient handoffs or transitions of care (33%), delays in treatment (31%), and increased patient complaints or dissatisfaction (30%).
Bill Schuh, CEO of Firstup, emphasized the systemic nature of these failures. “Nurses are doing everything they can to care for patients in incredibly demanding conditions, but they are being asked to navigate communication systems that were not designed for clinical environments,” he said. “When communication breaks down, the entire system breaks down, and any lapse can negatively impact patient care or lead to costly incidents.”
Beyond patient outcomes, communication failures are contributing to the healthcare workforce crisis. Eighty-eight percent of nurses said miscommunication from management caused workplace issues. The reported effects included increased stress or burnout (52%), a desire to leave their department or unit (32%), and even a desire to leave the profession altogether (21%). These retention pressures come at a time when healthcare providers worldwide are struggling with persistent staffing shortages.
Communication breakdowns also erode collaboration. Forty percent of nurses said miscommunication from management decreased teamwork within their units. Given that 50% of nurses receive important workplace updates directly from their managers, ineffective communication creates a cascade of operational and clinical challenges across entire departments.
Communication as Clinical Infrastructure
The Firstup research underscores that communication in healthcare cannot be treated as an administrative afterthought. The findings highlight communication as a core component of both engagement and clinical reliability.
For hospitals, the report suggests moving beyond traditional broadcast methods toward intelligent, personalized approaches that reach nurses where they are and when they need information. This involves rethinking not only how information is delivered but also the relevance, timing, and format of messages sent to frontline clinical staff.
As healthcare organizations continue to manage staffing shortages and burnout, improving communication effectiveness represents both a risk mitigation measure and an operational necessity. It supports compliance, reduces stress, strengthens collaboration, promotes retention, and ultimately protects patient care quality.